- Home
- Species
- Clostridioides difficile
Clostridioides difficile (Cdi)
Clostridioides difficile is Gram-positive species of spore-forming bacteria.
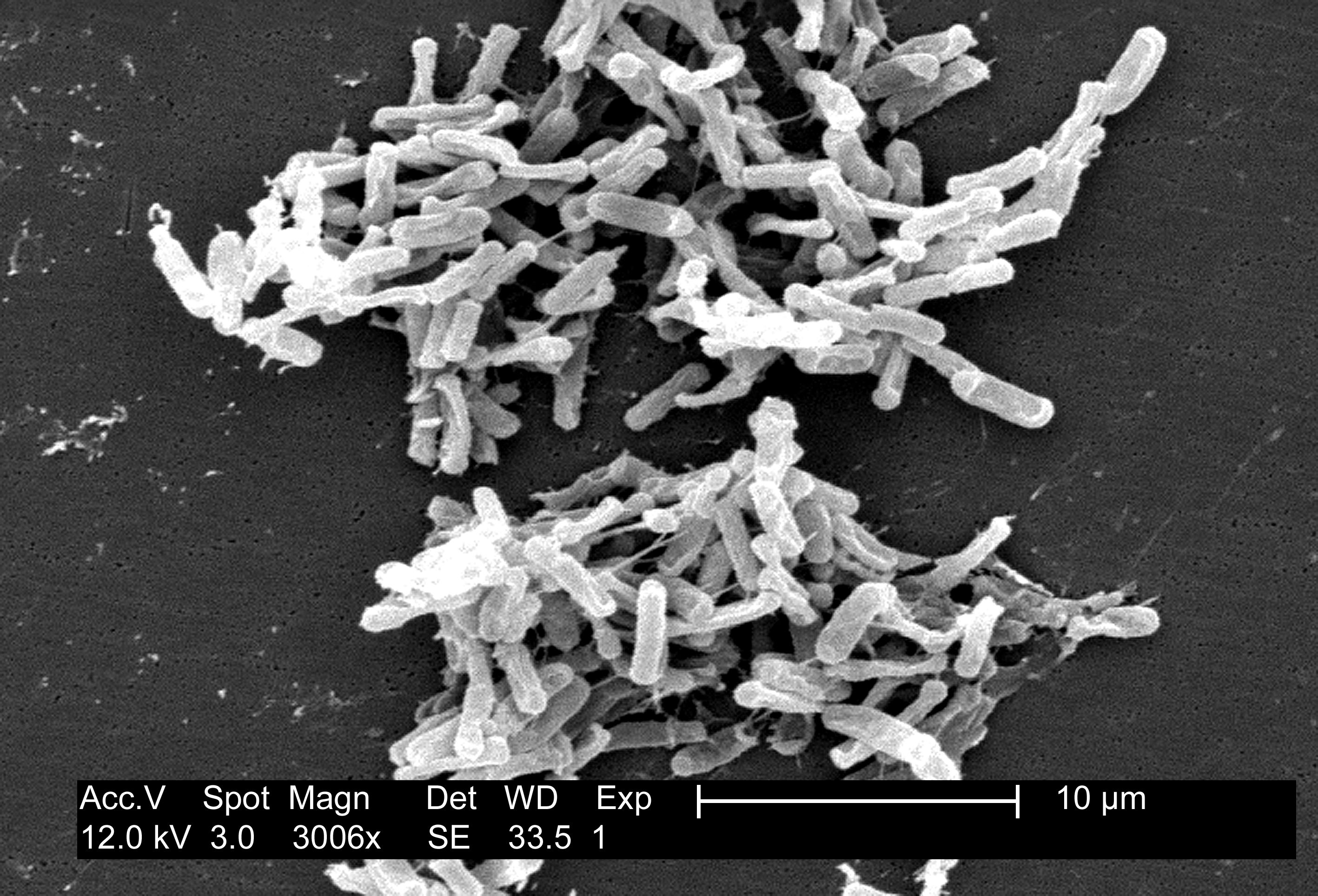
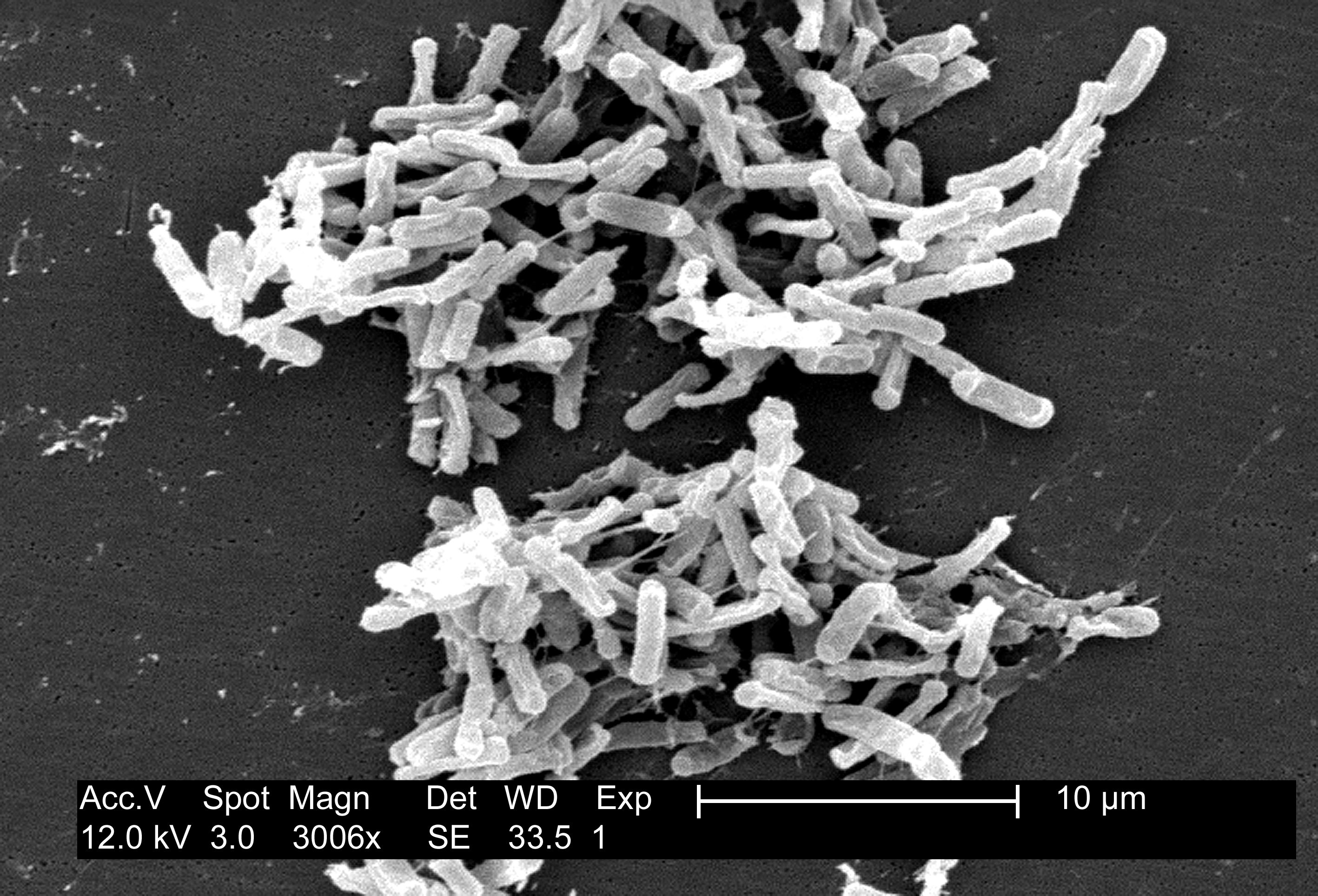
Clostridioides spp. are anaerobic, motile bacteria, ubiquitous in nature and especially prevalent in soil. Its vegetative cells are rod-shaped, pleomorphic, and occur in pairs or short chains. Under the microscope, they appear as long, irregular (often drumstick- or spindle-shaped) cells with a bulge at their terminal ends (forms subterminal spores). Under Gram staining,
C. difficile cells are Gram-positive and show optimum growth on blood agar at human body temperatures in the absence of oxygen.
C. difficile is catalase- and superoxide dismutase-negative, and produces two types of toxins: enterotoxin A and cytotoxin B, which disrupts cytoskeleton signal transductions in the host. Under stress conditions, the bacteria produce spores that are able to tolerate extreme conditions that the active bacteria cannot tolerate.
C. difficile is an important emerging human pathogen; according to the CDC, in 2017 there were 223,900 cases in hospitalized patients and 12,800 deaths in the United States. Although
C. difficile is commonly known as a hospital and antibiotic associated pathogen, at most one third of infections can be traced to transmission from an infected person in hospitals, and only a small number of antibiotics are directly associated with an elevated risk of developing a
C. difficile infection (CDI), namely clindamycin, fluoroquinolones and cephalosporins. The majority of infections are acquired outside of hospitals, and most antibiotics have similar elevated risk of infection on par with many non-antibiotic risk factors, such as using stool softeners and receiving an enema.
C. difficile can also become established in the human colon without causing disease. Although early estimates indicated that
C. difficile was present in 2–5% of the adult population, more recent research indicates colonization is closely associated with a history of unrelated diarrheal illnesses, such as food poisoning or laxative abuse. Individuals with no history of gastrointestinal disturbances appear unlikely to become asymptomatic carriers. These carriers are thought to be a major reservoir of infection. [From Wikipedia]